Understanding the Stages of Dermatomyositis: A Comprehensive Guide
Understanding the stages of dermatomyositis is essential for effective treatment and management of this complex autoimmune disease. This article discusses each stage and provides insights and guidance.
Understanding the stages of dermatomyositis is essential for effective treatment and management of this complex autoimmune disease. This article discusses each stage and provides insights and guidance.
Dermatomyositis (DM) is a complex autoimmune disease characterized by muscle inflammation and a characteristic rash. Although the disease can affect all ages, it is primarily diagnosed in adults between 40 and 60 years of age and children between 5 and 15 years of age. The disease includes a range of symptoms that often progress through different stages, making early detection and diagnosis essential for effective treatment and management. The course of dermatomyositis can be divided into different stages. Understanding these stages can provide insight into the evolution of the disease, the treatment required at each stage, and the impact on a patient's quality of life. This guide aims to provide a detailed overview of each stage from initial onset to possible complications, while emphasizing the importance of medical intervention and patient education.
Stage 1: Early Symptoms
The first stage of dermatomyositis usually marks the first onset of symptoms, which can range from mild to severe.
- The most obvious symptom of this stage is the appearance of a rash, commonly known as heliotrope rash, which can appear as purple or purplish discoloration of the eyelids or face. Patients may also develop Gottron papules, small, raised, erythematous lesions on the knuckles. These skin changes may be the first sign of dermatomyositis and prompt those affected to seek medical attention.
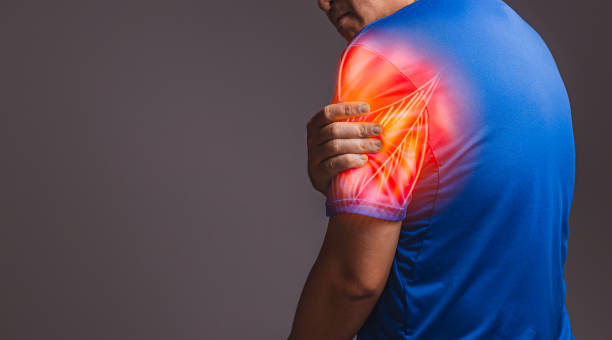
- In addition to skin symptoms, patients may also experience muscle weakness, although this symptom can sometimes be subtle. This weakness typically affects proximal muscles, such as those in the hips, shoulders, and neck, making daily activities difficult. Patients may find it difficult to lift objects, climb stairs, or perform overhead maneuvers. Recognizing these early symptoms is important because timely intervention can significantly alter the course of the disease.
- During the first stage, a healthcare provider will typically perform a thorough evaluation, including blood tests to check for elevated muscle enzymes and possibly a muscle biopsy to evaluate for muscle inflammation. These diagnostic tools help confirm the presence of dermatomyositis and rule out other conditions that may mimic its symptoms. Early diagnosis can lead to timely treatment, which is critical for long-term outcomes.
Stage 2: Acute Inflammation
- Stage 2of dermatomyositis is characterized by an escalation in symptom intensity that characterizes the acute inflammatory phase of the disease. During this stage, patients typically experience more pronounced muscle weakness, particularly affecting proximal muscles (such as the thighs, shoulders, and upper arms). This weakness can severely impact mobility and daily function, making tasks such as standing, walking, or lifting objects increasingly difficult. Muscle tenderness and pain may also increase, with patients often reporting deep aching discomfort.
- In addition to muscle symptoms, skin manifestations also become more pronounced, with worsening of the heliotrope rash and Gottron papules.
- In addition to these dermatologic signs, patients may also experience more general symptoms such as fever, fatigue, and unintentional weight loss. Laboratory tests typically show elevated muscle enzymes, including creatine kinase (CK), indicating muscle damage, while inflammatory markers such as C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) are often elevated, indicating systemic inflammation.
- In some cases, acute inflammation can also affect other organ systems, including the lungs, heart, or gastrointestinal tract, which can lead to complications such as interstitial lung disease, myocarditis, or gastrointestinal problems. Immediate intervention at this stage is critical to prevent further muscle damage and control systemic inflammation. Treatment typically includes corticosteroids (such as prednisone) and immunosuppressive medications, as well as physical therapy to treat muscle weakness and improve function.
Stage 3: Chronic Phase
Stage 3 of dermatomyositis marks the transition to the chronic phase where symptoms are stable but can last longer.
- During this stage, muscle weakness may stagnate, and although patients may not return to baseline strength, they can learn to adapt to decreased ability.This adjustment often includes physical therapy and rehabilitation, with an emphasis on maintaining mobility and function.
- During this stage, those affected often struggle with the psychological and emotional stress of a chronic condition. The unpredictability of flare-ups can lead to anxiety or depression as patients struggle with restrictions on physical activity and lifestyle. Support groups or counseling can play an important role in helping patients cope with the condition.
- In terms of treatment, treatment strategies in stage 3 may include the use of corticosteroids to control inflammation and immunosuppressants to modify disease progression. Regular follow-up with a healthcare provider is essential to monitor the effectiveness of treatment measures and adjust treatment regimens when necessary. The adjustment period may provide an opportunity to address any complications that may arise from long-term treatment, such as steroid-related side effects.
Stage 4: Complications May Emerge
Stage 4 raises awareness of the risk of complications associated with dermatomyositis.
- While some patients experience relief or improvement in their symptoms, others may experience ongoing problems or complications, including muscle wasting and difficulty breathing, which can seriously impact overall health.
- In some cases, dermatomyositis may be associated with an underlying malignancy, especially in adults, which has prompted increased screening in some patients. Patients at this stage should remain vigilant for possible complications. Lung problems, such as interstitial lung disease, may occur and require evaluation and monitoring with imaging and lung exams.
- Muscle weakness can also lead to complications such as falls or difficulty swallowing, which may require referral to a specialist, such as a physical therapist or speech therapist.
- Healthcare providers may consider additional interventions, including advanced imaging techniques and referrals for other treatment options, depending on the specific complications affecting the patient.A multidisciplinary approach, which may include a team of rheumatologists, dermatologists, physical therapists, and dietitians, is essential to optimize patient care at this stage.
Stage 5: Management and Treatment Strategies
Treatment of dermatomyositis is essential at all stages, but especially in the later stages, to improve quality of life and relieve symptoms.
- Treatment typically involves a combination of medications and supportive therapies aimed at controlling inflammation, improving muscle strength, and treating skin lesions. Corticosteroids are usually first-line therapy and may be combined with other immunosuppressants in more severe cases.
- In addition to medications, regular physical therapy is important to maintain muscle strength and function. A tailored exercise program can help maintain mobility, strength, and overall physical fitness. Given the potential for chronic fatigue, energy conservation strategies may also be beneficial for patients to manage daily activities.
- Patient education plays a vital role in the treatment of dermatomyositis. We encourage those affected to learn about the disease, its progression, and effective self-care strategies. This knowledge empowers patients to take charge of their health and make informed decisions in collaboration with their healthcare team. Additionally, understanding the importance of regular follow-up exams and monitoring is essential to detect relapses or complications early.
Establishing a collaborative relationship between patients and their care team can facilitate proactive management and improve overall outcomes. Ongoing research into dermatomyositis is revealing more about its pathophysiology, possible triggers, and new treatment options. As our understanding of this disease continues to evolve, we will hopefully find more targeted treatments that will improve outcomes and ultimately improve the lives of those affected by dermatomyositis.